In spite of CR rates of 75-80% currently achieved with anthracycline-cytarabine regimens in younger patients with favorable and intermediate-risk AML, relapse remains a major issue. The French AML intergroup launched the BIG-1 trial in 2015 in order to test different strategies aiming at reducing relapse rate and improving survival. All patients with previously untreated non-APL and non-CBF AML aged 18-60 years are eligible for trial participation which is still ongoing. The trial design includes several randomizations (R): Idarubicin vs daunorubicin for induction (R1), HDAC vs IDAC for consolidation (R2), post-transplant GVHD prophylaxis modalities (R3). R4 consists of nested randomized phase 2-3 trials testing the addition of new drugs to the IDAC or HDAC backbones during the consolidation phase. The protocol was designed to allow the sequential evaluation of several new agents over the trial period. Vosaroxin (VOS) has shown antileukemic activity (Advani, Clin Cancer Res 2010). The combination of VOS and IDAC showed higher CR rate and a non-significant OS benefit as compared to a placebo-IDAC arm in a large phase 3 trial in patients with refractory/relapsed AML (Ravandi Lancet Oncol 2015). We hypothesized that the addition of VOS to IDAC would improve LFS as compared to IDAC alone when given during the consolidation phase.
Methods. Eligibility criteria in the BIG-1 trial include: previously untreated AML according to WHO 2016 classification (AML secondary to an untreated myelodysplastic syndrome allowed), age 18-60, ECOG PS 0-2, no cardiac contra-indication to anthracyclines. Patients with APL and patients with CBF-AML are excluded. Eligibility criteria for R4 randomization were: Patients in first CR/CRp/CRi following 1 or 2 courses of induction chemotherapy according to the BIG-1 protocol; ELN2010 favorable- and intermediate-risk groups; ECOG PS ≤ 3; Absence of severe uncontrolled infection. Patients were scheduled to receive Cytarabine: 1.5 gr/m² twice daily on D1, 3, 5 with or without Vosaroxin: 70 mg/m² on D1 and D4 per cycle for a maximum of three cycles at 4-6 weeks intervals. Patients scheduled for allo-SCT or those who had reached CR after 2 induction cycles were to receive only 2 cycles of VOS-IDAC/IDAC.
R4-VOS sub-trial was designed to detect an increase of the 18-month LFS from 55% to 75% using a two-step phase 2-3 study. With type I and II errors set at 20% and using a one-sided test, 70 patients had to be randomized. If the predefined statistical objectives were met, study would resume recruiting 130 additional patients in the phase 3 part for a total of 200 patients.
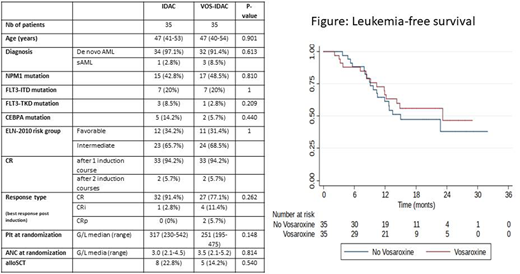
Results. 70 patients (35 in each arm), median age 47, ELN 2010 favorable and intermediate risk groups, have been included. 94% had de novo AML with NPM1 mutations in 46% and FLT3-ITD in 20%. As shown in the Table, patients and disease characteristics were not different between the 2 arms except for slightly more patients in CRi in the VOS-IDAC arm. Patients received a median of 4 chemotherapy cycle (including induction; range 3-4) without difference between the treatment arms. 13 patients (18.5%) received an alloSCT (VOS-IDAC: 5, IDAC: 8). Time between cycle 1 and cycle 2 was significantly longer in the VOS-IDAC arm (p= 0.017). Hematologic toxicity was higher in the VOS-IDAC group with a significantly longer neutropenia duration after each cycle, a greater number of RBC and Platelet transfusions, a significantly greater number of days with antibiotics and antifungal therapies and days with fever (during cycle 1). There were also significantly more cutaneous toxicity, mild nausea/vomiting and diarrhea in the VOS-IDAC arm.
With a median follow-up of 19 months, 14 and 15 patients relapse in the VOS-IDAC vs IDAC arms respectively. The study primary endpoint has not been reached and LFS was not significantly higher in the VOS-IDAC arm (18-month LFS of 51% vs 46% for VOS-IDAC vs IDAC respectively; see Figure) even after accounting for allo-SCT as a time-dependent variable (p-value=.49). The 2-year CIR was 51% vs 46% (p=NS) and 2-year OS was 88% vs 68% (p=NS).
Conclusion, the study's primary endpoint has not been met and results fail to show a significant improvement of 18-month LFS with the addition of VOS to IDAC consolidation of favorable/intermediate-risk AML in first CR. The phase 3 part of the trial will not open. The BIG-1 trial is still ongoing and uses the same design to tests addition of other drugs to the IDAC/HDAC consolidation backbone.
Guieze:abbvie: Honoraria, Other: advisory board, travel funds; janssen cilag: Honoraria, Other: advisory board, travel funds; roche: Other: travle funds; gilead: Honoraria, Other: travel funds; astrazanecka: Honoraria, Other: advisory board. Dombret:Pfizer: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; Nova: Consultancy, Research Funding; Celgene: Consultancy; Jazz Pharma: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Sunesis: Consultancy; Servier: Consultancy, Research Funding; Daiichi Sankyo: Consultancy; Astellas: Consultancy; Menarini: Consultancy; Janssen: Consultancy; Cellectis: Consultancy; Shire-Baxalta: Consultancy; Immunogen: Consultancy; Otsuka: Consultancy; Abbvie: Consultancy. Hunault:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Diachi: Membership on an entity's Board of Directors or advisory committees; Jansen: Honoraria; Servier: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal